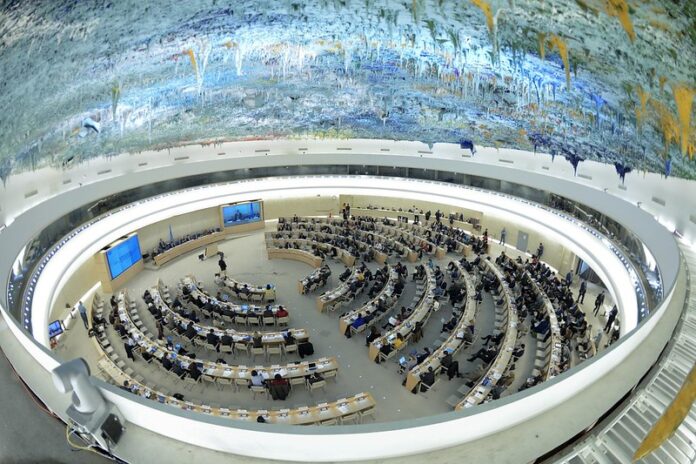
This blog was submitted by Dr. Katrina Perehudoff, Law Centre for Health and Rights at the University of Amsterdam, and Medicines Law & Policy, to the Office of the High Commission on Human Rights following an Expert Workshop on access to medicines
Persistent and new challenges to global access to medicines call for action by states, the private sector, and civil society for the enjoyment of human rights by all.
States bear the primary responsibilities for ensuring the conditions for universal access to medicines. Several steps are incumbent upon states.
First, states should enshrine in national law explicit individual rights and state obligations for access to medicines and set clear boundaries to these in line with human rights law. States should also establish clear pathways in domestic law for accountability and redress of medicines stock outs and high prices causing health rights violations. Some national UHC laws embed these components and are useful sources of inspiration for other lawmakers; however, there is still room for improvement. We have developed a rights-based checklist (that also serves as a wish list to guide legal reform) for evaluating the right to health components of a national pharmaceutical policy and domestic UHC laws with response to the affordability of and access to medicines.
Second, governments should establish a consistent practice of being transparent about how and how much public funds are spent on the R&D of medicines and the net prices paid to purchase them. This practice not only supports the right to health, but is also aligned with the right to access public documents and with the WHA Resolution 72.8 on transparency of pharmaceutical markets. UN Member States have the remit not to enter into confidentiality agreements with pharmaceutical companies if doing so is not in the public interest. Some Member States have adopted national legislation for greater transparency of R&D costs, and discounts, and rebates. For example, France and Italy have adopted laws requiring pharmaceutical manufacturers to disclose the public R&D investments in new medicines seeking reimbursement. States should also refrain from legitimizing confidential (purchase) arrangementswith pharmaceutical companies as part of domestic law. These examples should inspire legal reform elsewhere. A report by WHO Europe outlines further steps that states can take.
Third, governments should adopt measures in their national laws for sharing intellectual property, including patents, know-how and technology that are needed to guarantee the right to health. When other steps fail to yield medicines at affordable prices and sufficient quantities, states should be willing to use these legal measures at the national level to suspend exclusive rights and ensure affordability. Regulating the private sector for the realization of the right to health is an important state obligation. For that purpose, states need to ensure national implementation of the flexibilities contained in the WTO TRIPS Agreement in a manner that allows for the effective use of such flexibilities. States should also refrain from exerting pressure on countries that make use of TRIPS flexibilities in the public interest.
Fourth, a rights-based response requires states—working individually and cooperating globally—to finance biomedical R&D in the public interest and to equitably distribute the resulting goods. These actions are consistent with the rights to science and health. Alternative innovation models that have ‘access by design’ at their core are one example. Various UN resolutions and UN Special Rapporteurs (on health, culture) support medicines patent pooling.
Fifth, UN Member States should make every effort to advocate for equitable and affordable access to essential medicines in their positions as members of regional and international organizations, such as the European Union and WTO. Research indicates that states are inconsistently held to account by the UN CESCR for their actions regarding vaccine policy as members of international organizations. When acting as members of these organizations, states should act in line with the principle of systemic integration in international law, which requires in the case of pharmaceuticals that the TRIPS Agreement and United Nations human rights treaties be interpreted in harmony.
Although states bear the primary duty for the realization of human rights, the private sector and specifically the pharmaceutical industry, also bears important responsibilities. To this end, a welcome proposal is that for a global independent body for the accountability of the pharmaceutical industry, in line with those proposed by former UN Special Rapporteurs on the Right to Health.Civil society plays an important role in the transmission, uptake, and adherence to human rights norms by states and the private sector. Civil society is critical for the transmission of human rights principles and narratives to domestic policy debates and legal reforms, where they can shape state practices. Civil society is also critical for holding states and the private sector to account for their actions, such as through the Access to Medicines Index, the ‘Fair Pharma’ scorecard, access to price information requests, and signaling potential anticompetitive practices. Therefore, civil society groups acting in the public interest should be adequately resourced through public funds to avoid an over reliance on the private sector, which can create unwelcome conflicts of interest in pharmaceutical policy.